Wedoany.com Report on Feb 7th, The increasing complexity of healthcare services is driving the demand for timely and accurate access to health information at the point of patient care. Bedside health information network solutions have become a critical part of healthcare infrastructure, enabling real-time data exchange among care providers, systems, and different environments. These systems bridge gaps in information flow by delivering relevant data at the point of care to support clinical decision-making and improve patient outcomes.
 Healthcare systems are undergoing a significant transformation, placing greater emphasis on real-time data accessibility and integrated communication. Bedside health information networks have become essential tools in modern clinical settings, enabling healthcare professionals to access critical patient information directly at the point of care. Traditional centralized data systems are gradually being replaced by distributed networks that support mobility, flexibility, and rapid decision-making. The application scope of digital health platforms is expanding to outpatient clinics, emergency units, as well as rural and home environments, where immediate data access can directly impact clinical outcomes.
Healthcare systems are undergoing a significant transformation, placing greater emphasis on real-time data accessibility and integrated communication. Bedside health information networks have become essential tools in modern clinical settings, enabling healthcare professionals to access critical patient information directly at the point of care. Traditional centralized data systems are gradually being replaced by distributed networks that support mobility, flexibility, and rapid decision-making. The application scope of digital health platforms is expanding to outpatient clinics, emergency units, as well as rural and home environments, where immediate data access can directly impact clinical outcomes.
A notable trend in the industry is the move towards interoperability. Healthcare systems are actively investing in platforms that can seamlessly integrate with multiple electronic health record systems, diagnostic tools, and third-party applications. There is a growing demand for solutions that can consolidate data from diverse sources such as laboratories, imaging centers, pharmacies, and wearable devices. These trends are also driven by the concept of patient-centered care, which requires real-time updates, medication tracking, and care coordination across multidisciplinary teams.
The proliferation of cloud infrastructure is transforming how data is stored and transmitted in bedside networks. Cloud solutions support scalability and high availability, allowing healthcare institutions to scale their services more easily without being constrained by on-premise systems. Mobile compatibility and device integration are becoming increasingly important, as tablets, smartphones, and portable diagnostic tools have become central components of daily clinical operations. These developments reflect the industry's commitment to creating a more responsive, efficient, and interconnected health information environment.
Despite rapid progress in bedside health information network solutions, several operational challenges remain. Fragmentation of data across multiple systems can lead to inconsistencies in patient records and inefficient workflows. By implementing standardized data formats and interfaces, different systems can communicate more effectively. Application Programming Interfaces (APIs) and health information exchange protocols play a crucial role in facilitating this integration, enabling seamless data flow across platforms.
Data security remains a key concern, especially as the transmission of sensitive health information across networks increases. Concerns about unauthorized access, data breaches, and system vulnerabilities have driven the adoption of advanced encryption technologies, secure login protocols, and multi-factor authentication. These measures ensure that patient information is protected while authorized personnel can still access it in real time. Compliance with data protection regulations has been integrated into system design, enhancing trust and accountability among users.
Data overload is another challenge. Clinicians often face an overwhelming amount of information that may not be directly relevant to clinical decision-making. Bedside systems now incorporate features such as intelligent data filtering, prioritization tools, and context-aware alerts to help clinicians focus on actionable insights and avoid being distracted by irrelevant details, thereby improving decision efficiency and reducing cognitive burden.
Workflow disruptions during system implementation can hinder adoption, especially in environments unfamiliar with digital tools. Resistance to change and the learning curve associated with new technologies can delay the realization of benefits. Strategies to address this include integrating user-friendly interfaces, adaptive learning platforms, and role-based training programs. Involving clinical staff in system design and customization ensures that solutions align with daily workflows, enhancing usability and satisfaction.
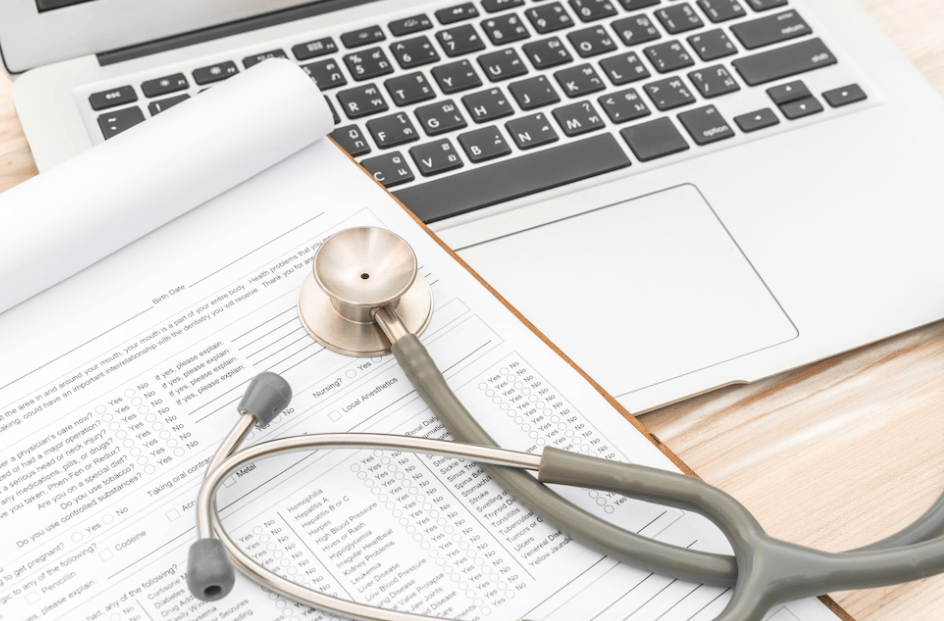
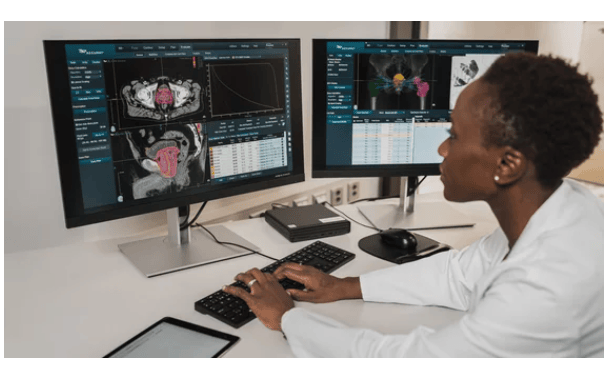
The development of bedside health information networks brings benefits to all parties in the healthcare continuum. For clinicians, the availability of accurate and timely data improves diagnostic quality, supports early intervention, and facilitates more precise treatment planning. Access to a patient's complete medical history, current medications, allergies, and laboratory results at the point of care reduces the occurrence of medical errors and enhances overall patient safety.
Patients also benefit from these solutions. Care continuity improves when all care team members can view and update patient records in real time. This promotes better coordination, particularly during transitions between different care settings. Transparency and accessibility of information encourage patients to actively participate in their health management, promoting adherence to treatment plans and increasing satisfaction.
Technological innovation continues to drive system expansion and value creation. Artificial intelligence and machine learning are increasingly being integrated into bedside systems to assist with diagnostic support, predictive analytics, and personalized care pathways. These technologies help predict complications, identify high-risk patients, and suggest evidence-based interventions, significantly enhancing clinical decision-making capabilities.
The integration of wearable devices and remote monitoring tools extends the functionality of bedside networks. These integrations allow for continuous data collection outside traditional clinical settings, enabling timely responses to physiological changes and improving chronic disease management. Healthcare providers benefit from richer datasets, while patients enjoy the convenience of remote care and reduced hospital visits.