Wedoany.com Report on Feb 7th, Clinical professionals often face issues such as fragmented systems, multiple logins, and cumbersome operations. Against the backdrop of increasing stress and professional burnout, the usability of Electronic Patient Record (EPR) systems is particularly crucial. Poorly designed systems not only affect efficiency and increase the burden on healthcare workers but may also pose risks to patient safety.
Enhancing EPR usability through change management is one of the key strategies. The experience of the Maidstone and Tunbridge Wells NHS Trust (MTW) digital projects indicates that the first step is to delve into the clinical frontline to understand actual workflows and challenges. Johanna Kelly points out: "Experience shows that our understanding of workflows often differs from reality. Clinical staff employ various workarounds to complete tasks." Therefore, digital workflow design should optimize clinical processes rather than impose restrictions.
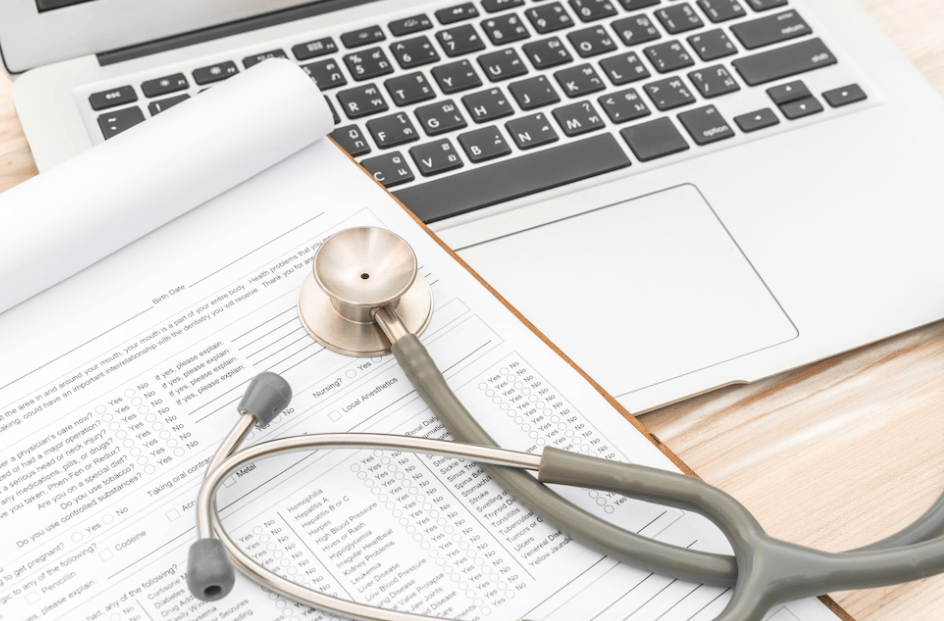
Establishing a clinically-led culture is equally important. Users can provide feedback on usability through channels such as working groups and dedicated email addresses. Simultaneously, incorporating usability testing into the change control process—for example, piloting in demonstration wards before gradual rollout—helps ensure the EPR system better aligns with actual needs.
Clinically-led, digitally-enabled design should become the norm. Mandating clinical staff participation in early decision-making and throughout the design process can better incorporate practical experience. Senior leadership support needs to be reinforced through clear actions and communication to drive an overall cultural shift. Currently, EPR implementation should be viewed as an organizational-wide initiative, not merely a technical project.
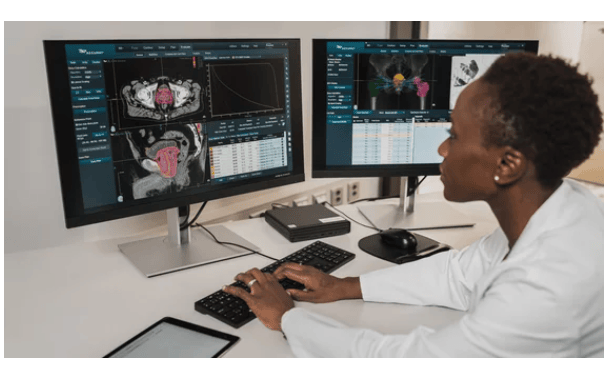
MTW achieved multiple usability improvements through flexible configuration of the EPR system. For instance, simplified specialty clinical documentation combining free-text boxes and form fields enhanced data collection efficiency and reduced documentation fatigue. The automatic vital signs entry function saves approximately 2.5 minutes per instance, nearly halving recording time and freeing up significant time annually for direct patient care. Furthermore, tag integration and patient context launch optimized system navigation, while clinical summary integration enhanced information retrieval efficiency.
EPR usability design is closely linked to patient safety. Issues such as complex interfaces, cumbersome logins, and poor information visibility can increase cognitive load and affect decision-making speed. Johanna Kelly emphasizes: "We have demonstrated that with the right tools and deep clinical engagement, processes can be optimized to make systems both easier for clinical use and beneficial for patients." Across the industry, there is a need to increase awareness of the connection between design and safety, promote a digital-first culture, and integrate data workflows into all activities.
Successful EPR deployment extends beyond system go-live; it requires continuous optimization. It necessitates collaboration among clinical, digital leadership, and technical partners, combined with a flexible and configurable platform, to truly enable efficient care. The ultimate goal is to achieve a clinically-led, digitally-enabled EPR system that alleviates the burden on healthcare workers and provides safer care for patients.