Researchers at Stanford School of Medicine have recently published study results in The Lancet, confirming that gene-engineered skin transplants can effectively treat chronic wounds in patients with dystrophic epidermolysis bullosa (EB). This therapy received U.S. Food and Drug Administration approval in April 2025, bringing new hope to patients with this rare genetic skin disease.

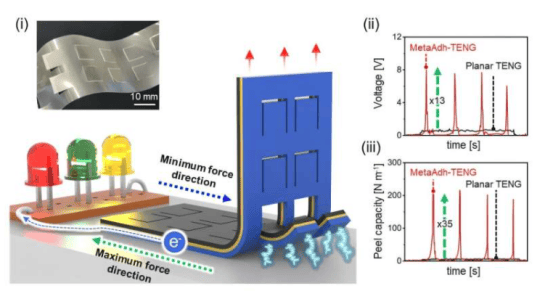
This phase 3 clinical trial was led by Jean Tang, MD, PhD, Professor of Dermatology at Stanford's Lucile Packard Children's Hospital, and involved 11 patients aged 6 and older. The team collected healthy skin samples from patients, introduced corrected COL7A1 genes using retroviruses in the laboratory, and cultured functional skin grafts. Study results showed that at 24 weeks post-transplant, 81% of treated wounds achieved at least 50% healing, significantly outperforming the 16% healing rate in the control group.
"This technology has successfully healed the most difficult-to-treat wounds, which are often the most painful areas for patients," said Dr. Tang. Charlotte Brown, a 20-year-old trial participant, stated: "The pain has noticeably decreased after the transplant, and my quality of life has improved significantly."
This therapy is the culmination of 20 years of research at Stanford School of Medicine, dating back to foundational work by Professor Paul Khavari's team in 2003. The technology has been licensed to Abeona Therapeutics for commercialization and will be rolled out at five hospitals nationwide.
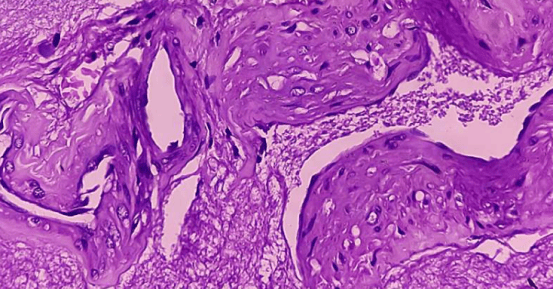
Patients with dystrophic epidermolysis bullosa suffer from skin blisters and wounds due to defects in type VII collagen. The research team will continue long-term follow-up of participants for up to 15 years to assess the durability of the transplanted skin.